A brief history of AKU's contribution to Pakistan's national vaccine programme
If you are a Pakistani who is protected from 12 deadly diseases—from Pneumonia to Typhoid—chances are that a research scientist from Aga Khan University's Department of Paediatrics & Child Health had something to do with it directly or indirectly.
Over the last 35 years, researchers from this one department alone, Paediatrics & Child Health, have been responsible for introducing four vaccines to Pakistan's Expanded Immunisation Program (EPI). They have also produced scientific evidence to persuade the government to switch to better versions of existing vaccines. And published studies to show how effective some vaccines are to help policymakers decide how to allocate resources on such preventive healthcare.
When the EPI started in 1978, it initially vaccinated Pakistan's children against six diseases. Then there was a two decade lull until AKU's Dr. Zulfiqar Bhutta and Dr. Anita Zaidi began their study of infectious diseases that were killing children.
.jpg)
It can take years to add a vaccine to the EPI list so children across the country receive it. First, researchers have to prove there is a significant burden of disease. Clinical trials need to investigate if a vaccine is effective. Researchers must then present this data to a government so it can decide if and how to introduce a vaccine.
And finally, the help of international organizations such as the WHO and Global Alliance for Vaccines and Immunisation (Gavi) is enlisted to help a country come up with ways to pay to roll out a new vaccine in the entire population.
This entire cycle brings together thousands of people from the field site staff who collect stool samples in places like Bhains Colony to the biostatistician who crunches the raw data at the AKU's Infectious Disease Research Lab. The funding for such large and prolonged research projects is won through competitive grants worth hundreds of thousands of dollars. But none of this would happen were it not for the spirit of the principal investigators or scientists who have made it their life's work. Here are some of their stories:
Typhoid
 It was in 1990 that Dr Zulfiqar Bhutta began studying Typhoid fever at AKU. At that time, Karachi did not have a lot of diagnostic laboratories and most people could not afford tests. So the goal was to study the signs and symptoms of Typhoid in children in order to create a formula that any doctor could use to easily diagnose it without expensive tests. The research was then expanded from the hospital into poorer parts of Karachi such as Sultanabad, Hijrat Colony, Sherpao Colony and Rehri Goth where children were most at risk.
It was in 1990 that Dr Zulfiqar Bhutta began studying Typhoid fever at AKU. At that time, Karachi did not have a lot of diagnostic laboratories and most people could not afford tests. So the goal was to study the signs and symptoms of Typhoid in children in order to create a formula that any doctor could use to easily diagnose it without expensive tests. The research was then expanded from the hospital into poorer parts of Karachi such as Sultanabad, Hijrat Colony, Sherpao Colony and Rehri Goth where children were most at risk.
Dr Bhutta enlisted the help of Dr Sajid Soofi who was a young doctor in those days. They ran 12-hour clinics at the hospital's research field sites starting with Bilal Colony. If anyone there had Typhoid, AKU did their tests and gave them free medicines. This grew into a campaign in which 60,000 schoolschildren were vaccinated with the then available Typhoid vaccine (a polysaccharide) in Karachi.
This was how the foundation for community-based research was laid at AKU. Researchers studying the burden disease at these field sites also treated families for free. This built trust and helped the community gradually understand the importance of vaccinations in the long run.
Meningitis
 By 2000, Dr Anita Zaidi came back from the US and joined the Department of Paediatrics & Child Health. She started screening children for meningitis because she realized that Pakistan's EPI did not vaccinate for it. Her team set up a system whereby hospitals and clinics sent their samples of Cerebrospinal fluid of any child who had a lumbar puncture if they were suspected of having meningitis.
By 2000, Dr Anita Zaidi came back from the US and joined the Department of Paediatrics & Child Health. She started screening children for meningitis because she realized that Pakistan's EPI did not vaccinate for it. Her team set up a system whereby hospitals and clinics sent their samples of Cerebrospinal fluid of any child who had a lumbar puncture if they were suspected of having meningitis.
The work expanded to different hospitals and communities in Karachi and Hyderabad. AKU tested for meningitis for free at its lab, which is how it was discovered that the bacteria called Haemophilus influenzae type B (Hib) was largely making these children sick. This research was done with the help of a WHO grant and AKU was able to show that Hib infection was a major problem in Pakistan, causing 20,000 deaths annually. With support from GAVI, Pakistan become the first developing country in Asia to include Hib in its vaccination program in 2006.
Later on, Pakistan became one of the first countries in Asia to introduce both the Haemophilus Type b (Hib) antigen containing Pentavalent vaccine (which also protects against diphtheria, tetanus, pertussis, and Hepatitis B), and the pneumococcus vaccines. The Pentavalent vaccine decreased the number of jabs for children from one for 3 diseases to one for 5 diseases.
 The pneumococcal vaccine was added to the EPI after AKU followed up with children who were diagnosed with severe pneumococcal meningitis. Researchers went to their homes 6 months later to learn what happened to them. It was devastating to see how many children died at home afterwards, the permanent disabilities they suffered from such as seizures, developmental delay, blindness and deafness.
The pneumococcal vaccine was added to the EPI after AKU followed up with children who were diagnosed with severe pneumococcal meningitis. Researchers went to their homes 6 months later to learn what happened to them. It was devastating to see how many children died at home afterwards, the permanent disabilities they suffered from such as seizures, developmental delay, blindness and deafness.
When this information was shared with the government it added the pneumococcal vaccine to the EPI.
Alongside this work, Dr Imran Nisar and Dr Fyezah Jehan were working on hospital-based pneumonia and its causes. Their work on pneumococcal carriage (how people carry it in their throats) and serotyping (classifying the type of bacteria) helped fast-track the introduction of the PCV 10 vaccine to the EPI in 2012. They also worked on establishing a superior efficacy of the 13-valent over the 10-valent vaccine.
 Similarly, once Pakistani leaders realized that 40% of diarrheal disease hospitalizations in young children were due to Rotavirus-induced dehydration and diarrhea, they wanted the vaccine introduced.
Similarly, once Pakistani leaders realized that 40% of diarrheal disease hospitalizations in young children were due to Rotavirus-induced dehydration and diarrhea, they wanted the vaccine introduced.
Polio
Between 2015 and 2018, the Department's researchers were involved in major evidence generation looking at the safety and immunogenicity of oral and injectable polio vaccine in newborns and children in Pakistan.
Dr Ali Faisal Saleem studied the safety of the polio vaccine, both oral and injectable, and which was the best timing for vaccinations to give children the best immunity (2018). This helped the government decide its routine and supplementary immunisation schedules. And Dr Fatima Mir worked on proving that it was safe to give babies the polio vaccine multiple times at different intervals (1 week, 2 weeks, 4 weeks).

As the world's focus shifted from giving children the Oral Polio Vaccine to an injectable one (iPV), AKU's faculty began studying the immune response to iPV in children and comparing results in malnourished versus well-nourished children. This is how it was established that a second dose of iPV was extremely important.
It is because of this work that AKU's researchers are asked to join international expert forums dealing with end-game polio eradication.
Rotavirus
Rotavirus is one of the most common viral pathogens that gives infants and children diarrhea and the best way to protect them is vaccination. In 2015, Dr Asad Ali, Dr. Momin Kazi and Dr. Anita Zaidi began studying how giving children the rotavirus vaccine prevented the diarrheal illness. This helped the government of Pakistan introduce it by 2017, making it the third time AKU's research informed policy at this level.
XDR Typhoid & Enteric infections
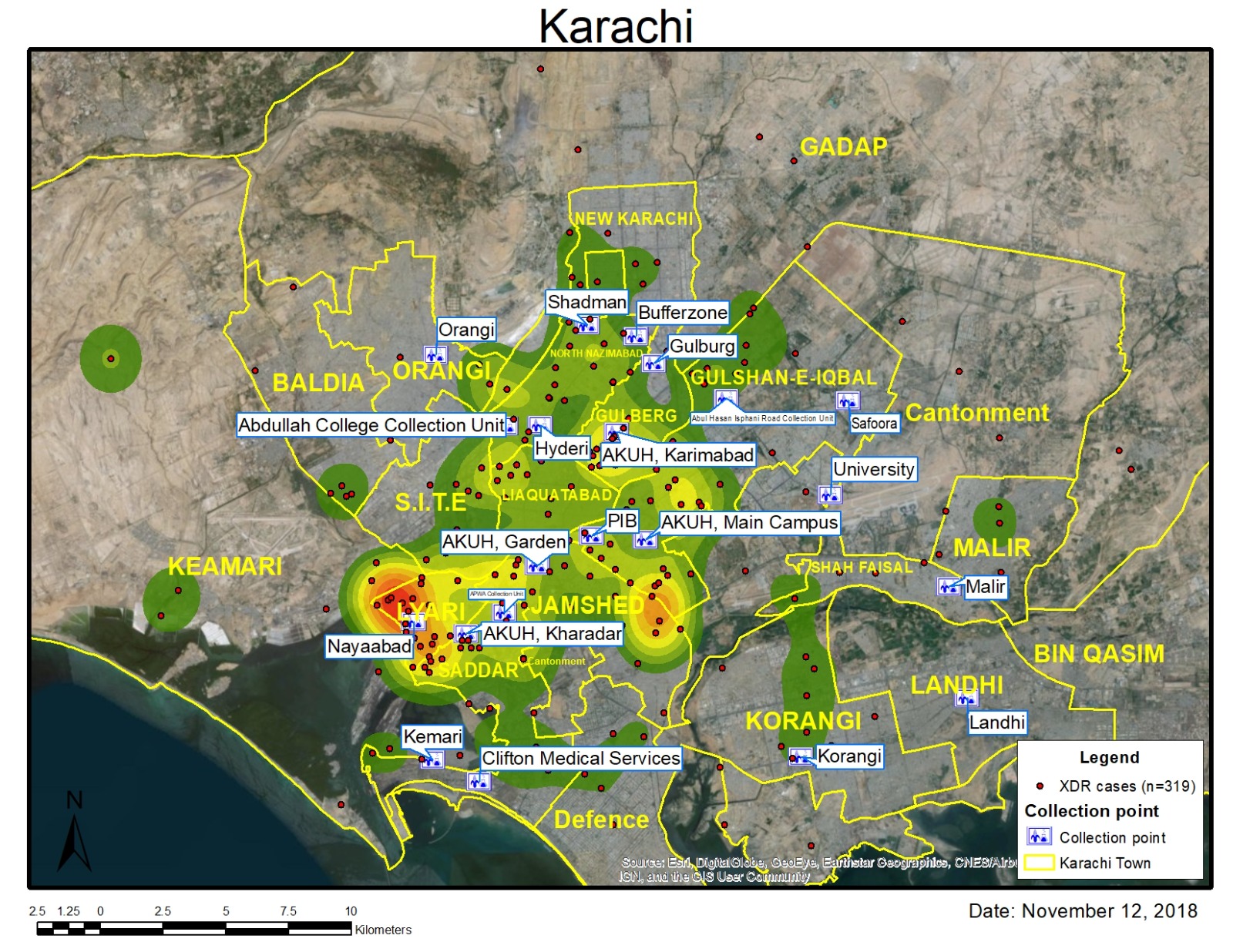 At around the same time, in 2017, there was an outbreak in Hyderabad of a mysterious Typhoid, which did not respond to the usual antibiotics. Dr. Farah Qamar, Dr. Tahir Yousufzai and Dr. Anita Zaidi discovered that this was the world's first case of Ceftriaxone-resistant Salmonella enterica serotype Typhi (Typhi). As a result of their research, the EPI added the Typhoid Conjugate Vaccine to its schedule by 2019. Prof. Farah Qamar was awarded the Tamgha-e-Imtiaz in recognition of this work.
At around the same time, in 2017, there was an outbreak in Hyderabad of a mysterious Typhoid, which did not respond to the usual antibiotics. Dr. Farah Qamar, Dr. Tahir Yousufzai and Dr. Anita Zaidi discovered that this was the world's first case of Ceftriaxone-resistant Salmonella enterica serotype Typhi (Typhi). As a result of their research, the EPI added the Typhoid Conjugate Vaccine to its schedule by 2019. Prof. Farah Qamar was awarded the Tamgha-e-Imtiaz in recognition of this work.
Upcoming projects
The work on vaccines continues at the Department of Paediatrics & Child Health. Some of our infectious disease experts more recently created systems to track primary immunodeficient children for the government's polio campaigns. Others are rolling out trials for vacccines to fight Hepatitis E, the cervical cancer-causing HPV infection and Malaria.


