Planting the Seeds of Learning in our Students: Workplace-based Assessment for Residency Program
This story is written by Lena Jafri, Assistant Professor, Department of Pathology and Laboratory Medicine, AKU
To me teaching is like gardening and my students are like plants. We, teachers, nurture our students, try to provide our students ideal environment to grow, and then watch them grow. Each student is unique with different needs. It is important for teachers to keep digging the soil and keep a check on the plant to help them reach their full potential. I introduced workplace-based assessment (WBA) in our residency program to foster my students, to keep a check on my students’ performance and how they will perform in future when independent.
Background
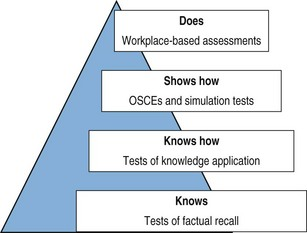
Recent trends in medical education are moving rapidly from scoring in high-stakes exams towards gathering evidence of clinical competence and professional behaviour observed in clinical environments. One of the most commonly used frameworks for assessing professional competence and skills is Miller's Pyramid (1). It has a series of levels of achievement beginning with knowledge (at the base) and ending with routine application in the clinical setting (at the top). The levels of Miller’s pyramid can be matched with assessment tools. While the written assessment is a tool at the ‘knows’ and ‘knows how’ levels; clinical assessment is at the ‘shows how’ level and patient outcomes and patient ratings are at the ‘does’ level. Similarly, I have used workplace-based assessment (WBA), a type of formative assessment that targets the highest level of the Miller’s pyramid (Figure 1), to collect information about my residents’ performance in their everyday practice.
Figure 1: WBA and Miller’s Pyramid
The objective of WBA in Chemical Pathology Residency
It was anticipated to:
- reinforce residents’ in-depth learning.
- help residents’ to overcome difficulties and improve performance.
- give regular feedback on performance.
- gauge residents’ ability to progress to the next level of residency.
WBA Process of Implementation
As the initial step WBA tool selection was done followed by outlining of the WBA process. Several hands-on workshops were conducted for faculty/ assessors to ensure WBA application in the field through role-playing. Multiple sessions for residents/students were held to explicate the purpose and process of WBA. A written WBA Guide was prepared and uploaded on Virtual Learning Environment (VLE) along with WBA tools for review and application.
Figure 2: Faculty development workshop on WBA

The WBA tools that were used to assess Chemical Pathology residents include Case-based discussion (CbD), directly observed practical skills (DOPS) and Evaluation of clinical events (ECE). For CbD the resident selects a case or procedure which he/she has recently been involved with and in whose notes they have made an entry or for whom they have reported results. Then he/she selects faculty as assessor and time. The discussion starts from, and is centred on the resident’s record in the notes or reports and is designed to assess clinical decision-making and the application or use of medical knowledge in the care of patients. The faculty completes the assessment form (CbD form) on VLE in the presence of the resident soon after the discussion and feedback. The assessments are performed against the standards expected at the end of the resident’s current stage of training. In short, the WBA process is resident-driven and the success of the WBA program is resident dependent. Repeated motivation and reminders were sent in the first few weeks to the Post-graduates (PGs) to get the ball rolling. While discussing with the groups of PGs, it was highlighted that the outcome is self-driven and rests on the individual PG. In essence, the selection of cases is PGs are responsible to select the cases and then approach the assessor for assessment and feedback.
Figure 3: Residents discussing cases and performing procedures as WBA activity
Lessons Learnt
1. Despite the challenges and limited resources, a high level of satisfaction among my faculty and PGs was observed. From my experience, I feel that faculty development, PGs’ meticulousness and administrative support are important factors that may influence the implementation and delivery of WBA in any other residency program within or outside Aga Khan University.
2. It is obvious, and quite understandable, that students are particularly sensitive to assessment. With the introduction of WBA in our residency program, my PG trainees are given feedback regularly leading to a positive impact on their learning and performance.
3. It gives the PGs more opportunity to interact with the faculty more often than before.
4. WBA created a learning opportunity for my PGs and improved the overall teaching-learning environment in the section.
5. It motivated the trainees to study more and in-depth.
6. The implementation of WBA has provided educational impact and good opportunities for feedback to PGs.
Conclusion
The WBA implementation provided the opportunity to connect teaching, learning, assessment and feedback. It gave the PGs opportunity to interact with assessors more often and learn from their rich experience. Complex professional attributes that are difficult to assess in written assessments, it can now easily be assessed through WBA by our faculty. Some attributes that can now be assessed via WBA are communication and consultation skills, practising metabolic medicine holistically, data gathering and interpretation, procedural skills, making a diagnostic decision, evaluation of clinical events, maintaining an ethical approach to practice and working in teams.
A Way Forward
Further steps are been taken to align it with the national curriculum of chemical pathology residency program from the College of Physicians and Surgeons of Pakistan and make the process acceptable at a national level.
Acknowledgements
I would like to thank my team of faculty, residents, senior technologists & manager of the section of Chemical Pathology, Department of Pathology and Laboratory Medicine; IT Academic Computing Department of AKU; Foundation for Advancement of International Medical Education and Research (FAIMER) fellows and faculty; TEL Champion Group Team of AKU and special thanks to AKU’s Scholarship of Teaching and Learning (SoTL) Grant for the financial support and guidance.
Reference:
Miller G. E. (1990). The assessment of clinical skills/competence/performance. Academic medicine:
Journal of the Association of American Medical Colleges, 65 (9 Suppl), S63–S67.
https://doi.org/10.1097/00001888-199009000-00045