Scoring Systems in Diagnosis of Disseminated
Intravascular Coagulation
Dr Natasha Ali,
Haematology
The liver is the most important organ involved
in the regulation of haemostasis. Most of the
clotting factors, their inhibitors and a number of
proteins responsible for fibrinolysis are produced
in the liver. Therefore, liver disease impacts both
primary and secondary haemostasis pathways
through a number of different mechanisms.
Abnormalities of the clotting cascade are the
predominant features of acute and chronic liver
disease. In some patients suffering from hepatic
disease, physicians are faced with the diagnostic
challenge of an underlying bleeding or thrombotic
diathesis due to overlap between various clinical
syndromes including Disseminated Intravascular
Coagulation (DIC). According to the International Society of Thrombosis
and Haemostasis (ISTH), DIC is a syndrome
characterised by a systemic intravascular activation
of coagulation, with loss of localisation, arising from
different causes. It can originate from and cause
damage to the microvasculature, which if suffi ciently
severe can produce organ dysfunction. ISTH also
proposed that the working defi nition of DIC can be
divided into two phases:
a) Non-overt DIC: represents subtle haemostatic
dysfunction
b) Overt DIC: de-compensated phase of non-overt
DIC. Events responsible for DIC in liver disease include
liver necrosis, impaired endotoxin clearance,
surgery, shock and ascites recirculation. DIC can
be recognised as a syndrome suggested by clinical
signs and laboratory tests. The characteristic
laboratory findings include: prolonged prothrombin
time (PT), activated partial thromboplastin time
(APTT), thrombin time (TT), increased levels
of fibrin related markers (fibrin degradation
products, D-Dimer), decreased platelet count,
fibrinogen level, plasma coagulation factors and
their inhibitors. More specialised and useful tests
include: prothrombin activation fragments and
thrombin-antithrombin complex (TAT).
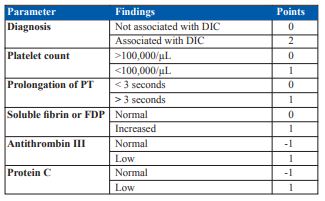
In 2001, ISTH proposed two separate scoring
systems for overt and non-overt DIC. The overt
DIC score consists of a fi ve steps diagnostic
algorithm, in which a specifi c score, refl ecting the
severity of the abnormality found, is given to each
of the laboratory tests [Table 1]. 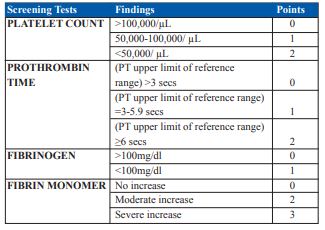
A score of fi ve or more is considered to be
compatible with DIC, whereas a score of
less than five may be indicative (but not
affirmative) for non-overt DIC.
Similarly using
certain clinical and laboratory findings [Table
2] a score of five or greater is compatible with non-overt DIC and could diagnostically define
patients with a poor prognosis due to haemostatic
dysfunction, independent of developing overt
DIC.
Following steps are suggested for the diagnosis
of DIC:
Step 1: Determine if the patient has an
underlying condition associated with DIC. If no
underlying is present then do not proceed further.
Step 2: Order screening coagulation tests and
decide whether patient has overt or non-overt
DIC.